Bilateral oophorectomy- A New risk factor for dementia
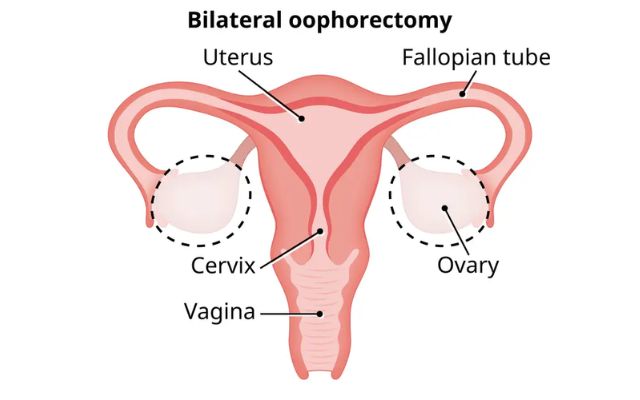
Bilateral oophorectomy, the surgical removal of both ovaries, is often recommended for women with a high genetic risk of ovarian cancer.
As medical science continues to advance, we discover new insights into the complexities of the human body. One such revelation has been the potential link between a surgical procedure called bilateral oophorectomy and the development of dementia. Bilateral oophorectomy involves the removal of both ovaries and is typically performed for various medical reasons. This article delves into the world of bilateral oophorectomy and explores the emerging evidence that suggests it may be associated with an increased risk of dementia. We’ll break down the procedure, the role of the ovaries, and the latest research findings, allowing you to make informed decisions about your health.
Understanding Bilateral Oophorectomy
Bilateral oophorectomy is a surgical procedure in which both ovaries are removed from a woman’s body. Ovaries are a pair of small, almond-shaped organs located in the lower abdomen, and they play a pivotal role in a woman’s reproductive and overall health. This procedure is often performed in conjunction with a hysterectomy, which is the removal of the uterus. There are various reasons why a healthcare provider might recommend bilateral oophorectomy, and it is essential to understand them:
- Cancer Prevention: Women with a high genetic risk of ovarian cancer, such as those with BRCA gene mutations, may opt for bilateral oophorectomy as a preventive measure. Removing the ovaries substantially reduces the risk of developing ovarian cancer.
- Gynecological Conditions: In cases of severe endometriosis, pelvic inflammatory disease, or persistent cysts or tumors on the ovaries, a healthcare provider might recommend bilateral oophorectomy to alleviate symptoms and improve a patient’s quality of life.
- Hormone-Related Conditions: Some conditions, such as polycystic ovary syndrome (PCOS) or hormone-sensitive breast cancer, may be treated by removing the ovaries. This helps reduce the production of hormones that exacerbate these conditions.
- Reproductive Choices: In some cases, women who have completed their families may choose to have their ovaries removed as a method of contraception.
While bilateral oophorectomy can offer health benefits in certain situations, it also has significant implications for a woman’s long-term health. The procedure induces surgical menopause, leading to an abrupt decline in estrogen and progesterone hormones, which can have far-reaching effects on various bodily systems.
The Role of Ovaries in a Woman’s Health
Understanding the role of the ovaries is essential to comprehend the potential implications of their removal. Ovaries are central to a woman’s reproductive system and play vital roles in hormone regulation and overall well-being:
- Hormone Production: Ovaries are responsible for producing estrogen and progesterone, two hormones critical for menstrual cycle regulation, bone health, heart health, and maintaining the elasticity of the skin.
- Reproductive Function: Ovaries store and release eggs, enabling women to conceive and bear children.
- Bone Health: Estrogen, produced by the ovaries, helps maintain bone density. A decrease in estrogen levels can lead to bone loss, which can eventually result in osteoporosis.
- Cardiovascular Health: Estrogen also has a protective effect on the cardiovascular system by maintaining healthy blood vessel function and regulating cholesterol levels.
- Brain Function: Emerging evidence suggests that estrogen may have neuroprotective properties, impacting cognitive function and mood.
The Link Between Bilateral Oophorectomy and Dementia
Research over the past few years has unveiled a potential link between bilateral oophorectomy and an increased risk of dementia. Dementia is an umbrella term for cognitive decline, with Alzheimer’s disease being the most common form. Let’s delve into the studies and findings that have shed light on this connection:
1. The Cache County Study (2007): One of the early studies to raise this concern was the Cache County Study, which investigated the relationship between bilateral oophorectomy and dementia in a large population. The study suggested that women who had undergone bilateral oophorectomy before menopause were at a higher risk of developing dementia than those who had not.
2. Timing Matters: Timing appears to be a crucial factor. Women who had the procedure before reaching natural menopause seemed to face a more substantial risk. It is hypothesized that the sudden hormonal changes brought on by surgical menopause may affect brain health over time.
3. Hormone Replacement Therapy (HRT): While the removal of the ovaries can lead to hormonal imbalances, the use of hormone replacement therapy (HRT) may mitigate some of these effects. HRT involves the administration of synthetic hormones to replace those lost due to oophorectomy. However, the impact of HRT on dementia risk is still a subject of research and debate.
4. Estrogen’s Neuroprotective Effects: Estrogen, produced by the ovaries, is believed to have neuroprotective properties. It plays a role in maintaining cognitive function, and a sudden drop in estrogen levels may affect brain health. Researchers are exploring whether estrogen therapy post-oophorectomy can reduce dementia risk.
5. Genetic Factors: Genetic factors may also play a role. Some individuals may have a genetic predisposition that makes them more susceptible to the neurological effects of hormone fluctuations.
6. Ongoing Research: It’s important to note that this field of research is continually evolving, and scientists are conducting further studies to gain a more comprehensive understanding of the relationship between bilateral oophorectomy and dementia.
Balancing the Scales: Weighing the Risks and Benefits
The potential link between bilateral oophorectomy and dementia is undoubtedly a matter of concern, but it should not overshadow the valid medical reasons for the procedure. Women facing a decision regarding oophorectomy should consider several factors:
- Individual Risk: Assess your personal risk factors, including family history, genetic predisposition, and the specific medical reasons for the procedure.
- Consult a Healthcare Provider: Discuss the potential risks and benefits of bilateral oophorectomy with your healthcare provider. They can provide guidance tailored to your situation.
- Alternative Options: In some cases, there may be alternative treatments or risk reduction strategies that can help avoid the procedure.
- Hormone Replacement Therapy: If you undergo bilateral oophorectomy, discuss the possibility of hormone replacement therapy with your healthcare provider. They can help you make an informed decision regarding HRT based on your medical history and the potential benefits and risks.
- Lifestyle Factors: A healthy lifestyle, including regular physical activity and a balanced diet, can have a positive impact on bone health and overall well-being.
FAQ
1. What is bilateral oophorectomy, and why is it performed?
Bilateral oophorectomy is a surgical procedure in which both ovaries are removed from a woman’s body. It is performed for various medical reasons, including cancer prevention, treating gynecological conditions, managing hormone-related issues, and, in some cases, as a method of contraception.
2. What roles do the ovaries play in a woman’s health?
The ovaries have multiple essential roles, including producing hormones like estrogen and progesterone, regulating the menstrual cycle, supporting reproductive function, maintaining bone health, and contributing to cardiovascular health and brain function.
3. How is dementia linked to bilateral oophorectomy?
Research has suggested a potential link between bilateral oophorectomy and an increased risk of dementia, particularly in women who undergo the procedure before natural menopause. The abrupt hormonal changes associated with surgical menopause, including a significant drop in estrogen, may impact brain health over time.
4. Does timing matter when it comes to dementia risk after bilateral oophorectomy?
Yes, timing appears to be a significant factor. Women who have the procedure before reaching natural menopause seem to face a higher risk of developing dementia. The sudden hormonal changes during surgical menopause may influence cognitive health.
5. Can hormone replacement therapy (HRT) mitigate the dementia risk associated with bilateral oophorectomy?
While HRT can help manage some of the hormonal imbalances resulting from oophorectomy, its impact on dementia risk is still a subject of research. Scientists are exploring whether estrogen therapy post-oophorectomy may reduce the risk of dementia.
6. Are genetic factors involved in the link between oophorectomy and dementia?
Genetic factors may also play a role in a woman’s susceptibility to the neurological effects of hormone fluctuations. Some individuals may have a genetic predisposition that makes them more vulnerable.
7. What should women consider when facing a decision regarding bilateral oophorectomy?
Women should assess their individual risk factors, consult with a healthcare provider to discuss the potential risks and benefits of the procedure, explore alternative treatment options, consider the potential of hormone replacement therapy, and maintain a healthy lifestyle to support overall well-being.
8. What is the ongoing research focusing on regarding the link between bilateral oophorectomy and dementia?
Ongoing research aims to gain a more comprehensive understanding of the relationship between oophorectomy and dementia. Scientists are investigating the impact of hormone replacement therapy, genetic factors, and the long-term cognitive effects of the procedure.
9. Should women avoid bilateral oophorectomy altogether to prevent dementia?
The decision to undergo bilateral oophorectomy should not be based solely on the potential dementia risk. Women should carefully evaluate the medical necessity, consider alternative options, and engage in discussions with healthcare providers to make informed choices about their health.
10. How can women balance the potential risks and benefits of bilateral oophorectomy?
Women can balance the scales by considering their individual risk factors, consulting healthcare providers, exploring alternatives, discussing the possibility of hormone replacement therapy, and maintaining a healthy lifestyle. The decision should be well-informed and tailored to individual needs.
Conclusion
The link between bilateral oophorectomy and an increased risk of dementia is a topic of growing interest in the medical community. While research is ongoing, it’s essential for women to be informed about the potential implications of this surgical procedure on their long-term health. The decision to undergo bilateral oophorectomy should be made based on a comprehensive evaluation of individual risk factors, medical necessity, and discussions with healthcare providers. In the end, balanced decision-making will ensure that women receive the most appropriate and personalized care while safeguarding their cognitive health. As science continues to unravel the complexities of the human body, these insights will empower women to make the best choices for their overall well-being.



